Understanding Tubal Reversal Surgery: Procedure, Benefits, and Expectations
Tubal reversal surgery, also known as tubal ligation reversal, is a significant medical procedure that offers hope to women wishing to conceive after having undergone a tubal ligation. This surgical intervention involves the reconnection of the fallopian tubes, which can restore natural fertility in individuals who have previously chosen to permanently sterilize themselves. As societal norms around family planning evolve and personal circumstances change, more women are exploring this option, making it imperative to understand the intricacies of the procedure, its benefits, and the realistic expectations surrounding it. This article delves into the various aspects of tubal reversal surgery, including the surgical techniques employed, potential risks and complications, and the factors influencing success rates. Additionally, we will explore the emotional and psychological implications of the decision to undergo this procedure, as well as the importance of consulting with qualified medical professionals. By providing a comprehensive overview, we aim to equip readers with the knowledge necessary to make informed decisions about their reproductive health and family planning options, ultimately helping them navigate the complexities of tubal reversal surgery with confidence and clarity.
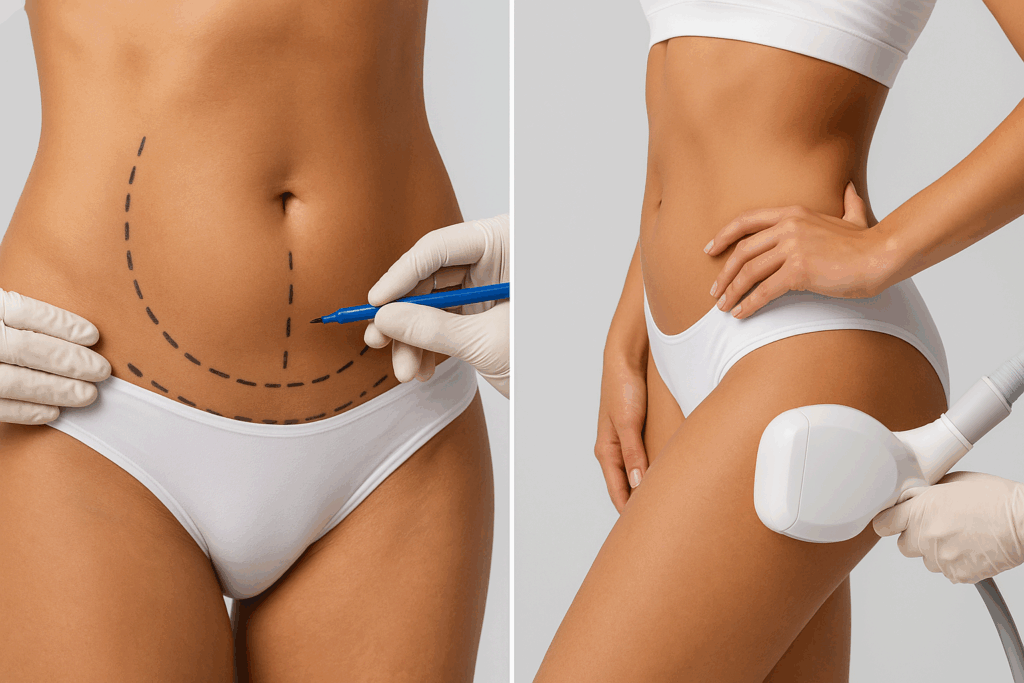
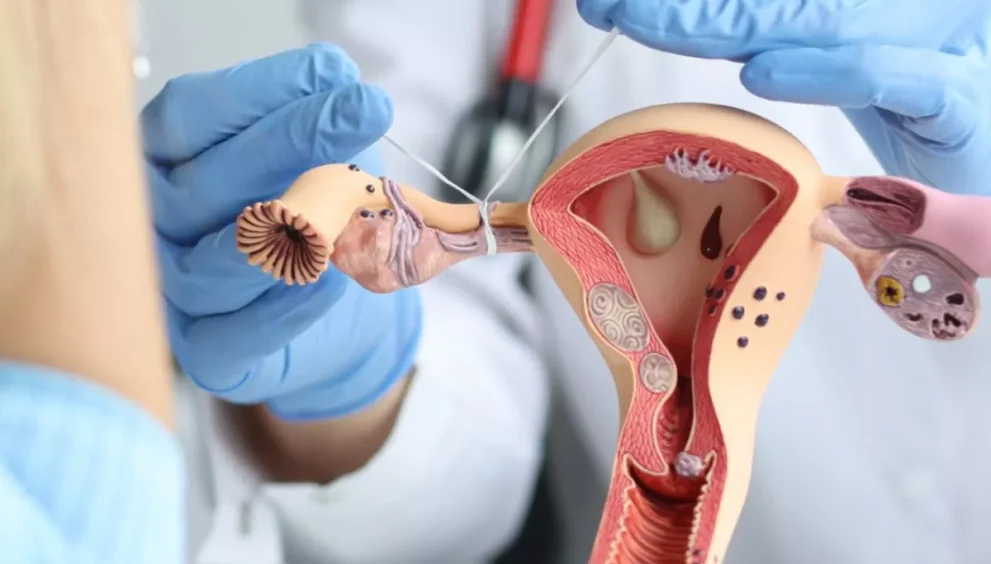
Overview of Tubal Reversal Surgery Procedure
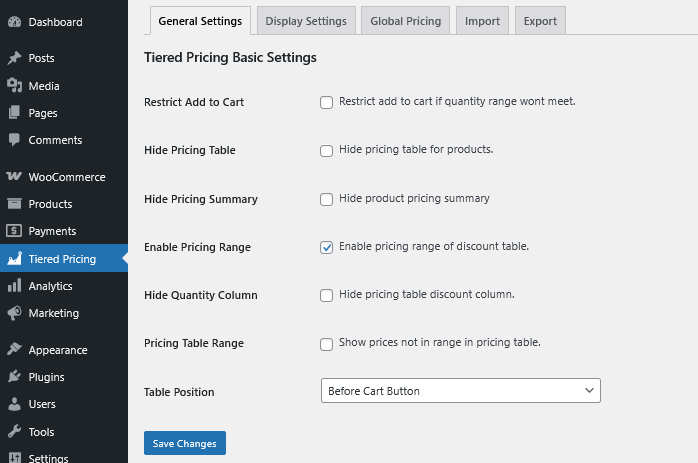
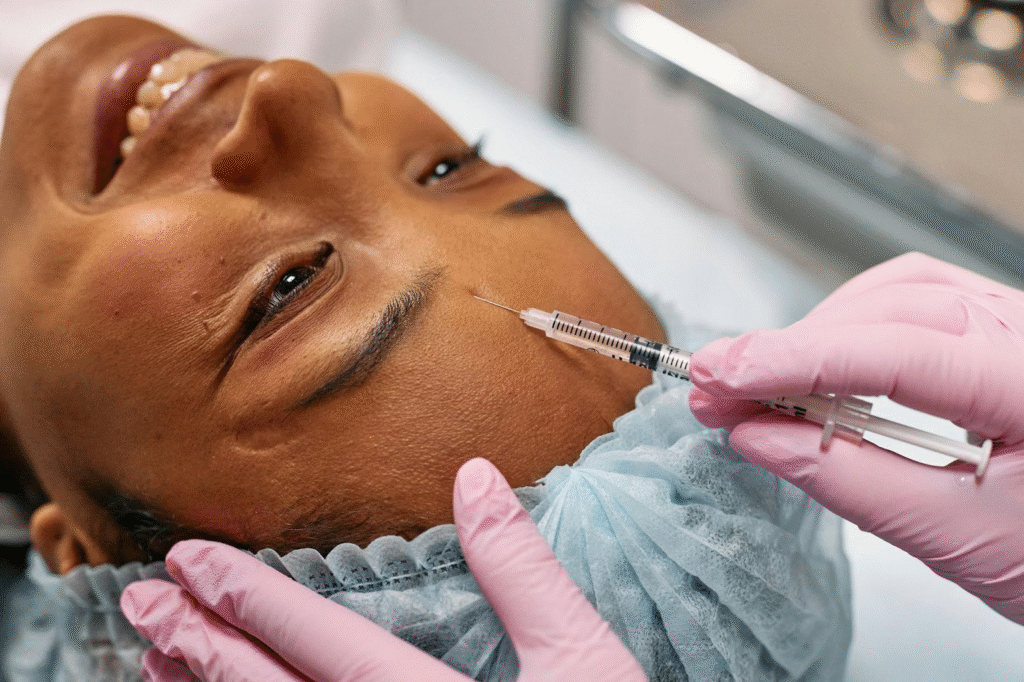
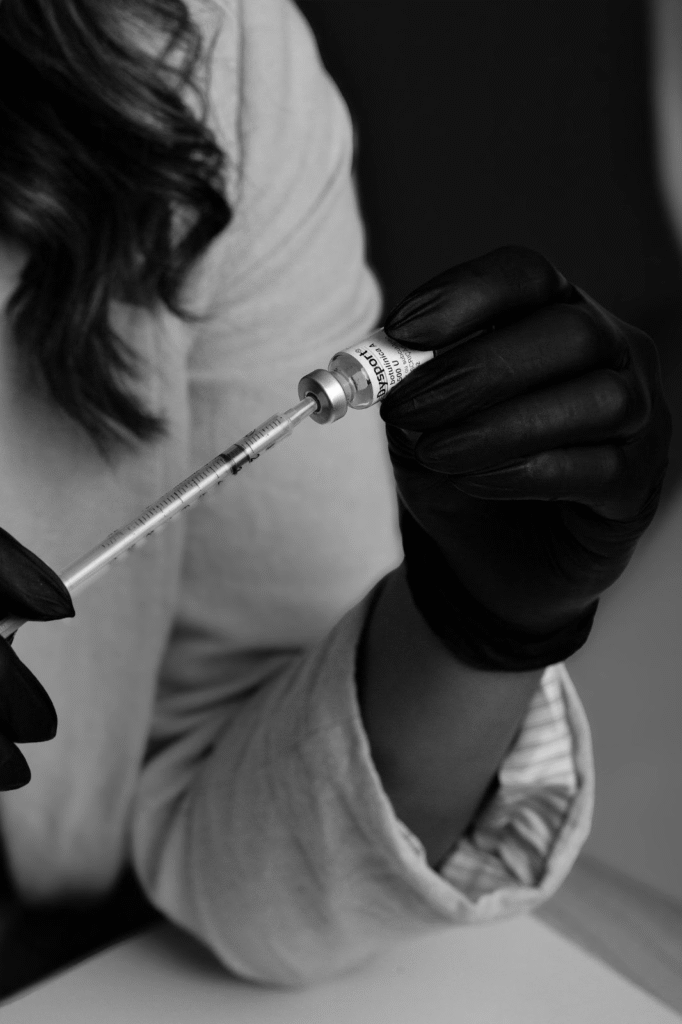
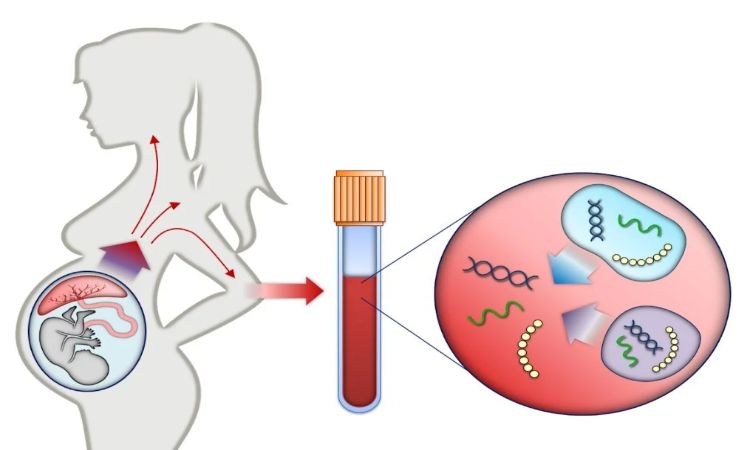
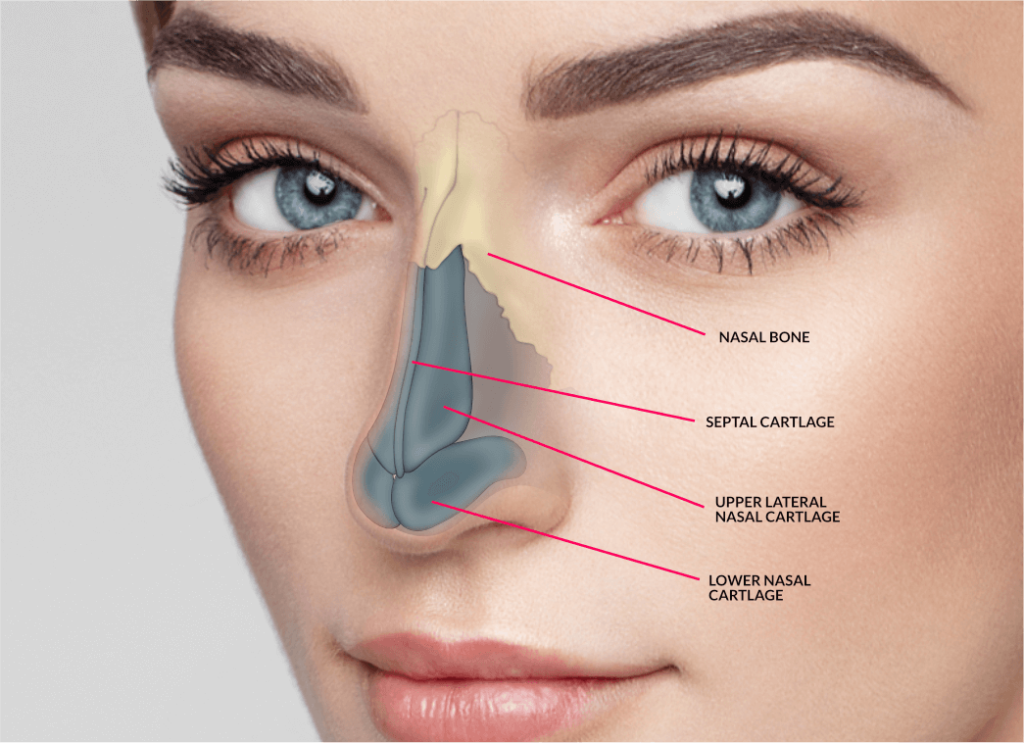
Tubal reversal surgery, also known as tubal reanastomosis, is a surgical procedure designed to restore fertility in women who have previously undergone tubal ligation. The surgery involves rejoining the fallopian tubes that were cut, tied, or blocked, thereby allowing for the possibility of natural conception. Typically performed under general anesthesia, the procedure can be carried out through either an open abdominal approach or laparoscopy, which is a minimally invasive technique that uses small incisions and a camera to guide the surgeon. The choice of method may depend on the patient’s specific circumstances, the surgeon’s expertise, and the extent of tubal damage.
During the operation, the surgeon carefully removes the blocked or damaged segments of the fallopian tubes and meticulously reconnects the healthy ends. Success rates for the procedure can vary based on several factors, including the woman’s age, the method of previous tubal ligation, and any underlying reproductive health conditions. Following the surgery, patients may be advised to wait for a period before attempting to conceive, with many experiencing improved chances of pregnancy compared to those who remain without intervention. Regular follow-up care is essential to monitor recovery and address any complications that may arise postoperatively.
A concise explanation of the surgical process involved in tubal reversal.
The surgical process for tubal reversal involves several critical steps to ensure the successful reconnection of the fallopian tubes. Initially, the procedure commences with an assessment of the pelvic anatomy, often utilizing laparoscopy to visualize the tubes, ovaries, and surrounding tissues. Once the surgeon identifies the condition of the fallopian tubes, they proceed to excise the damaged segments if necessary. This is followed by a meticulous reconnection of the healthy portions, utilizing fine sutures to align and secure the tubes in their appropriate positions, thereby restoring the pathway for sperm to meet the egg.
Post-surgery, patients are monitored for recovery and may require follow-up visits to ensure proper healing and evaluate the procedure’s success. While most women can expect a relatively quick recovery, complete healing of the reproductive system may take several months. Success rates are influenced by individual factors, including age, overall reproductive health, and the specifics of the previous tubal ligation, making personalized consultations essential for prospective patients.
Key Benefits of Tubal Reversal
One of the primary advantages of undergoing tubal reversal is the restoration of natural fertility, allowing women to attempt conception without the need for assisted reproductive technologies. By reestablishing the connection between the ovaries and uterus, the procedure enables the natural passage of eggs and sperm, thereby increasing the likelihood of pregnancy. This can be particularly appealing for those who desire more children after previously opting for sterilization.
Additionally, tubal reversal can lead to a more cost-effective approach to family planning compared to in vitro fertilization (IVF), which often requires multiple cycles and significant financial investment. Patients may also experience a sense of empowerment and control over their reproductive choices, as the procedure allows for the possibility of pregnancy at their discretion. Overall, the benefits of tubal reversal extend beyond physical health, encompassing emotional and financial dimensions that contribute to a fulfilling family life.
Highlights the advantages of undergoing tubal reversal for fertility restoration.
The procedure also presents a relatively low-risk option for restoring fertility, as it is typically performed laparoscopically, resulting in smaller incisions, reduced recovery time, and minimal postoperative discomfort. Furthermore, many women who undergo tubal reversal report high satisfaction rates, with studies indicating favorable success rates for achieving pregnancy, especially in younger patients. This option provides a viable pathway for women who wish to expand their families without the complexities associated with assisted reproductive technologies.
Moreover, the emotional benefits of tubal reversal should not be overlooked. Many women express a renewed sense of hope and optimism about their fertility journey, as the procedure symbolizes a second chance at motherhood. This emotional uplift can have a profound impact on overall well-being, fostering a positive outlook and reducing anxiety related to fertility challenges. Ultimately, tubal reversal not only restores physical capability for conception but also empowers women to reclaim their reproductive autonomy and fulfill their family aspirations.
Preparing for Surgery and Recovery
Preparation for surgery involves several key steps to ensure a smooth experience and optimal recovery. Patients should consult closely with their healthcare provider to discuss medical history, current medications, and any potential risks associated with the procedure. It is advisable to undergo preoperative tests, such as blood work and imaging studies, to assess overall health and readiness for surgery. Additionally, patients are often instructed to avoid certain medications, like blood thinners, and to refrain from eating or drinking for a specified period prior to the surgery. Setting up a comfortable recovery environment at home and arranging for assistance during the initial days post-surgery can further enhance the recovery experience.
Postoperative care plays a crucial role in the recovery timeline. Patients are generally encouraged to rest and gradually increase their activity levels as tolerated. Monitoring for any signs of complications, such as excessive pain or unusual discharge, is essential, and following the surgeon’s postoperative instructions will help facilitate a smooth healing process. Maintaining a healthy diet and staying hydrated can also support recovery. Emotional support from family and friends can provide encouragement and help manage any anxiety that may arise during this transitional period. This comprehensive approach to preparation and recovery can significantly impact overall outcomes and the patient’s journey towards achieving their family goals.
Important expectations for pre-operative preparation and post-surgery recovery timeframes.
e bleeding, severe pain, or signs of infection, is essential during the recovery period. Most individuals can expect to return to light activities within a week, but full recovery may take several weeks, depending on the complexity of the surgery and the patient’s overall health. Adhering to follow-up appointments and maintaining open communication with the healthcare team can help address any concerns that arise during the recovery process. Additionally, patients should be aware of the importance of a balanced diet and hydration to support healing, as well as the need to avoid strenuous activities until cleared by their surgeon.
Expectations for recovery can vary significantly based on individual circumstances, but a timeline can generally be established. Initial discomfort and swelling are common and typically improve within a few days. Patients should be prepared for gradual improvements, with most able to resume normal activities within four to six weeks. It is crucial for patients to listen to their bodies and not rush the recovery process, as proper healing is vital to achieving the best outcomes following the surgery.
In conclusion, understanding tubal reversal surgery is crucial for individuals considering this procedure as a means to regain fertility after tubal ligation. By comprehensively assessing the procedure, its benefits, and realistic expectations, patients can make informed decisions that align with their reproductive goals. While tubal reversal can offer renewed hope for many, it is essential to consult with a qualified healthcare provider to discuss individual circumstances and potential outcomes. With the right information and support, patients can navigate this journey with confidence, paving the way for a potential expansion of their family in the future.