How Health Economics Outcomes Research Informs Value-Based Healthcare Decisions

Healthcare systems worldwide face the dual challenge of improving patient outcomes while controlling costs. Rising expenditures, limited resources, and increasing demand for quality care have prompted the adoption of value-based healthcare models, which prioritize patient outcomes relative to the cost of care. Health economics outcomes research (HEOR) plays a critical role in supporting these models by providing evidence-based insights that guide decision-making. By evaluating clinical effectiveness, economic impact, and patient-reported outcomes, health economics outcomes research helps healthcare organizations, policymakers, and providers make informed choices that maximize value for patients and the system as a whole.
Understanding Health Economics Outcomes Research
Health economics outcomes research is a multidisciplinary field that combines clinical evidence, economic analysis, and patient-centered data to assess the value of medical interventions. It encompasses cost-effectiveness analysis, cost-utility analysis, budget impact modeling, and real-world evidence studies. HEOR examines not only the direct costs of treatments but also the broader implications, including hospitalization rates, productivity losses, and quality of life. By providing a comprehensive view of the benefits, risks, and costs associated with healthcare interventions, HEOR supports informed decision-making and facilitates the transition to value-based care.
The Shift Toward Value-Based Healthcare
Traditional fee-for-service healthcare models reward volume over outcomes, often resulting in fragmented care and escalating costs. Value-based healthcare, on the other hand, emphasizes outcomes, efficiency, and patient satisfaction. Providers and organizations are incentivized to deliver high-quality care that achieves measurable improvements in health while managing costs. This approach requires robust evidence to determine which interventions provide the greatest benefit relative to their cost, and this is precisely where HEOR contributes. By quantifying the clinical and economic impact of therapies, HEOR enables stakeholders to prioritize interventions that deliver optimal value.
Key Components of HEOR
HEOR integrates several analytical components to evaluate healthcare interventions. Cost-effectiveness analysis compares the costs and outcomes of competing treatments, typically using metrics such as quality-adjusted life years (QALYs) or incremental cost-effectiveness ratios (ICERs). Cost-utility analysis further examines the trade-offs between cost and the quality of life improvements associated with treatments. Budget impact models estimate the financial implications of adopting new interventions within a healthcare system, helping administrators and payers plan for resource allocation. Real-world evidence studies, derived from electronic health records, registries, and observational data, provide insight into how interventions perform outside of controlled clinical trial settings. Collectively, these tools enable a comprehensive understanding of value across clinical, economic, and patient-centered dimensions.
Informing Clinical Decision-Making
HEOR provides critical insights for clinicians when selecting treatment options. By evaluating both clinical efficacy and economic impact, healthcare providers can make evidence-based decisions that optimize patient outcomes while considering resource constraints. For example, two medications may be equally effective in managing a chronic condition, but HEOR might reveal differences in hospitalization rates, adherence patterns, or total cost of care. Clinicians can use this information to recommend interventions that deliver superior overall value, supporting the goals of value-based care while improving patient satisfaction and health outcomes.
Supporting Payer and Policy Decisions
Healthcare payers and policymakers also rely on HEOR to make informed coverage and reimbursement decisions. Economic evaluations help determine whether the benefits of a treatment justify its cost, ensuring that limited resources are allocated efficiently. HEOR informs formulary decisions, pricing strategies, and reimbursement policies, promoting interventions that provide meaningful improvements in health outcomes at sustainable costs. By integrating economic and clinical evidence, HEOR ensures that value-based healthcare systems reward interventions that truly enhance patient care.
Patient-Centered Outcomes
A cornerstone of HEOR is its focus on patient-reported outcomes and experiences. Evaluating quality of life, functional status, and satisfaction enables a more holistic understanding of the value of healthcare interventions. By incorporating patient perspectives, HEOR ensures that decisions reflect outcomes that matter most to individuals. For instance, a treatment may improve survival but negatively impact daily functioning or well-being; HEOR helps identify these trade-offs and supports decisions that align with patient priorities. This patient-centered approach strengthens the alignment of healthcare delivery with the goals of value-based care.
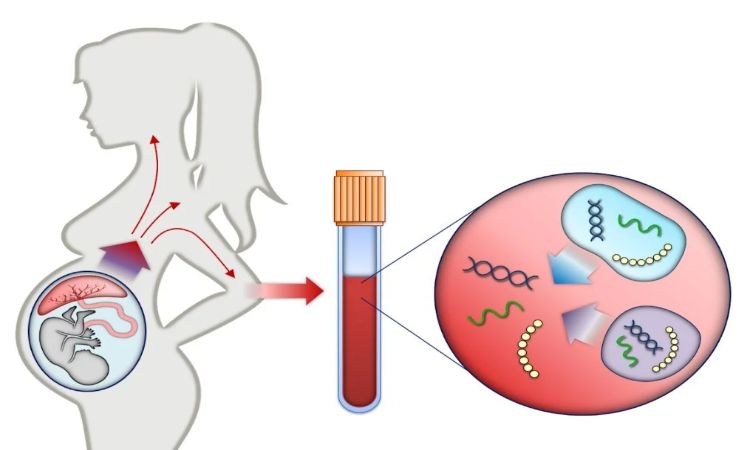
Real-World Evidence and Its Impact
While clinical trials provide controlled evidence of efficacy and safety, real-world data is essential for understanding how interventions perform in everyday practice. HEOR leverages electronic health records, registries, claims data, and observational studies to assess treatment effectiveness, adherence, and utilization patterns across diverse patient populations. This information helps identify variations in outcomes, potential cost savings, and areas for improvement, guiding the design of programs that enhance the efficiency and quality of care. Real-world evidence thus complements traditional clinical research, bridging the gap between trials and practical application.
Challenges and Limitations
Despite its value, HEOR faces several challenges. Data availability and quality can limit the accuracy of analyses, while differences in methodology may yield variable results. Economic models often require assumptions that may not fully capture real-world complexity, and translating findings into actionable policy can be difficult. Moreover, aligning incentives across providers, payers, and patients is essential for successful implementation of value-based strategies. Addressing these challenges requires continuous improvement in data collection, methodology, and stakeholder engagement.
Integration With Technology and Analytics
Advancements in technology are enhancing the role of HEOR in value-based healthcare. Data analytics platforms, machine learning algorithms, and predictive modeling enable more precise assessment of costs, outcomes, and patient trajectories. These tools facilitate personalized evaluations, allowing healthcare systems to tailor interventions to subgroups most likely to benefit. Digital health technologies, including remote monitoring and wearable devices, provide real-time data that informs economic and outcomes analyses, supporting adaptive strategies that respond to evolving patient needs and system pressures.
Driving System-Level Improvements
By providing evidence on the relative value of interventions, HEOR contributes to broader system-level improvements. Healthcare organizations can identify inefficiencies, prioritize high-impact interventions, and design programs that improve population health while controlling costs. Value-based contracting, bundled payment models, and accountable care initiatives are strengthened by robust HEOR data, ensuring that financial incentives align with patient outcomes. This systemic perspective allows stakeholders to implement policies and practices that optimize care delivery across the continuum.
The Role of Academic and Research Institutions
Academic and research institutions play a pivotal role in advancing HEOR methodologies and applications. By conducting rigorous studies, developing innovative analytical tools, and training the next generation of health economists, these institutions contribute to evidence-based decision-making in healthcare. UNT Health exemplifies this model by integrating health education, health research, and health care to support initiatives that generate actionable HEOR insights. Collaboration between researchers, clinicians, and policymakers enhances the impact of HEOR on real-world healthcare decisions.
Future Directions in HEOR
The future of HEOR is closely linked to the continued evolution of value-based healthcare. Emerging areas such as personalized medicine, digital therapeutics, and artificial intelligence offer new opportunities for evaluating and optimizing interventions. Integration of patient-generated data, genomics, and predictive analytics will refine assessments of value, enabling more precise and individualized healthcare strategies. Additionally, global collaboration and standardized methodologies will expand the applicability of HEOR, supporting healthcare systems worldwide in achieving sustainable, high-quality care.
Conclusion
Health economics outcomes research is a cornerstone of value-based healthcare, providing the evidence needed to make informed, patient-centered, and cost-conscious decisions. By combining clinical, economic, and patient-reported data, HEOR informs treatment selection, policy development, and system-level improvements. Its focus on both effectiveness and efficiency ensures that resources are used wisely while maximizing patient outcomes. Institutions like UNT Health Fort Worth highlight the importance of integrating research, education, and care to advance HEOR and value-based strategies. As healthcare systems continue to prioritize outcomes relative to cost, HEOR will remain an essential tool in shaping policies, guiding clinical decisions, and achieving sustainable improvements in health.