4 Ways Clinics Can Save Time and Boost Care Quality

Clinics today face the dual challenge of managing heavy administrative workloads while striving to deliver the highest quality of patient care. Juggling appointments, patient records, billing, and follow-ups can consume valuable time that could otherwise be dedicated to clinical duties. Finding ways to streamline operations is no longer just an advantage—it’s a necessity for a thriving practice. This article explores four effective strategies that clinics can implement to save time, increase efficiency, and elevate the standard of care they provide to their communities.
1. Streamline Appointment Scheduling and Management
The front desk is often the busiest area in any clinic, with staff handling a constant flow of phone calls for appointments, cancellations, and reschedules. This manual process is not only time-consuming but also prone to human error, leading to double-bookings or missed appointments. can revolutionize this workflow. Patients can book, change, or cancel their appointments online at their convenience, freeing up staff to focus on in-person patient needs. Automated reminders sent via text or email can significantly reduce no-show rates, which a study in the Medical Group Management Association (MGMA) Connection found can be as high as 5-7% on average. By automating these tasks, clinics can ensure a smoother patient flow and a more organized daily schedule, directly translating to more time for quality patient interaction.
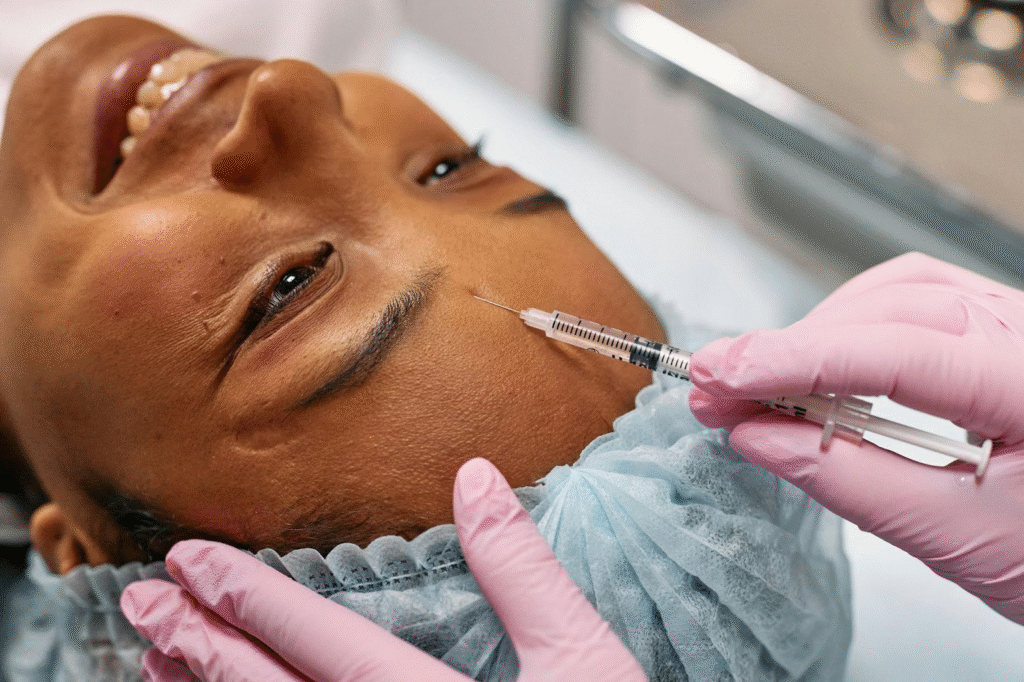
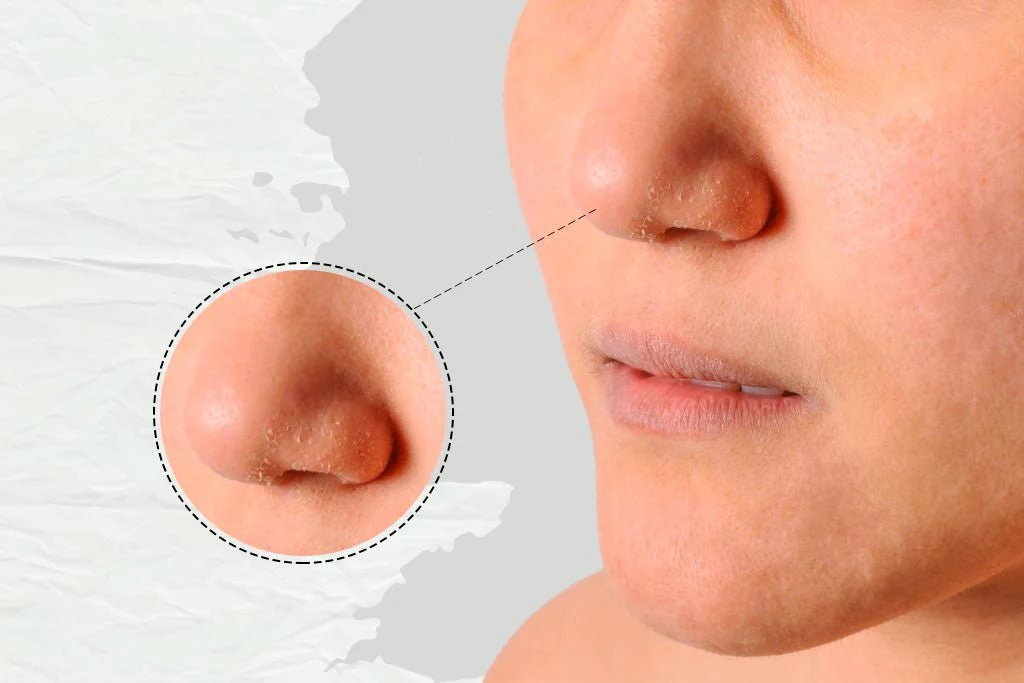
2. Optimize Clinical Documentation Processes
Accurate and thorough documentation is the backbone of quality healthcare, but it is also one of the most time-intensive tasks for clinicians. Physicians can spend nearly half of their workday on administrative tasks, with a significant portion dedicated to updating patient records. To combat this, clinics can adopt an electronic medical record system that offers customizable templates and voice-to-text transcription. These features allow doctors to capture patient information quickly and consistently during a visit, rather than spending hours after clinic closes.
Centralizing patient data in a digital format also means instant access to a patient’s history, allergies, and previous treatments, enabling faster and more informed decision-making during consultations. This not only saves precious minutes per patient but also enhances diagnostic accuracy and continuity of care.
3. Enhance Inter-Departmental Communication
Inefficient communication between different departments—such as the front desk, nursing staff, and billing office—can lead to significant delays and frustrations for both staff and patients. Misplaced lab results, delayed billing inquiries, or unclear instructions can create bottlenecks that disrupt the entire clinic’s workflow. Implementing a secure, internal messaging platform allows for real-time communication and seamless information sharing.
For example, a clinician can instantly notify the front desk when a patient is ready for checkout or send a query to the billing department without leaving their office. This eliminates the need for staff to walk around the clinic searching for information or playing phone tag. A study on clinical communication found that using secure messaging tools can reduce the time it takes to get a response by over 30%, fostering a more collaborative and efficient work environment.
4. Automate Billing and Claims Management
The financial health of a clinic depends on a timely and accurate billing process, but it is often a complex and tedious administrative function. Manual billing is fraught with potential errors, from incorrect coding to missed claim submissions, which can lead to denials and delayed payments. Automating the revenue cycle management process can drastically reduce these issues. Modern practice management software can automatically verify patient insurance eligibility, generate clean claims with accurate medical codes, and track their status in real time. By automating claim scrubbing and submission, clinics can improve their first-pass claim rate, which the MGMA recommends should be 95% or higher. This not only ensures a healthier cash flow but also frees up administrative staff from the burdensome task of chasing payments and reworking denied claims, allowing them to focus on more patient-centric financial counseling and support.