Understanding the Level 4 Office Visit CPT Code: Requirements and Reimbursement Tips

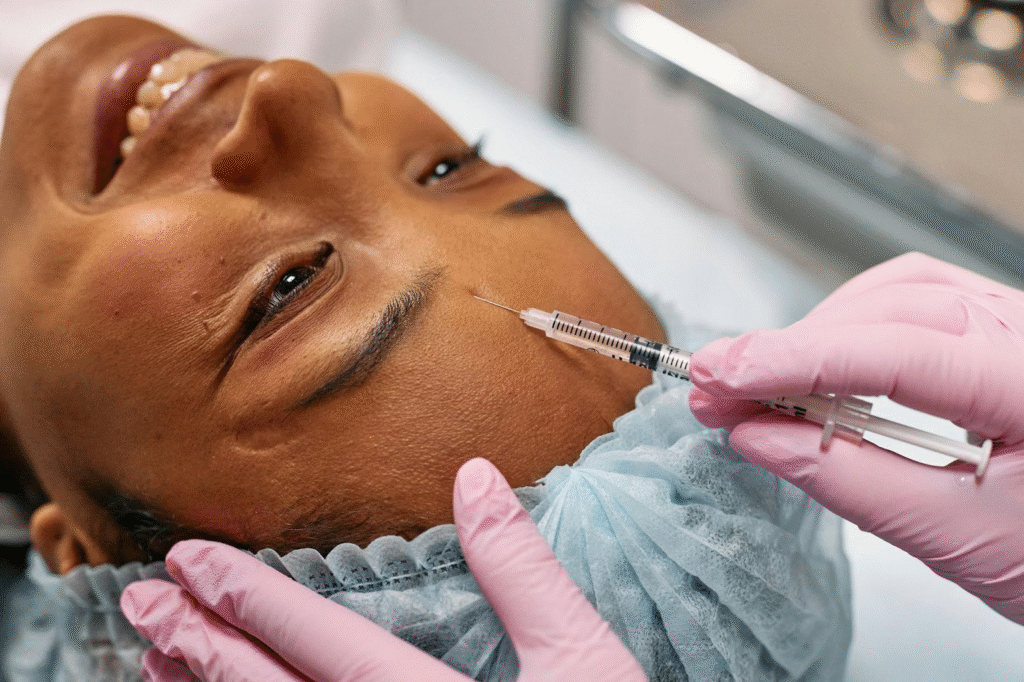
In the realm of medical coding and billing, the accurate documentation and classification of office visits are crucial for ensuring appropriate reimbursement and compliance with regulatory standards. One of the most commonly utilized codes in this context is the Level 4 Office Visit CPT Code, which corresponds to a comprehensive encounter requiring a high level of medical decision-making. Understanding the intricacies of this code is essential for healthcare providers, coders, and billing specialists alike, as it directly impacts revenue cycles and the overall financial health of medical practices. This article aims to demystify the requirements associated with the Level 4 Office Visit CPT Code, outlining the factors that contribute to its correct application—from patient history and examination details to the complexity of medical decision-making. Additionally, we will provide invaluable reimbursement tips that can assist practices in maximizing their claims while minimizing the risk of denials or audits. By equipping healthcare professionals with this knowledge, we hope to enhance their ability to navigate the complexities of coding, ultimately leading to more efficient billing processes and better patient care outcomes.
– Key Requirements for Level 4 Office Visit CPT Coding
The Level 4 Office Visit CPT coding requires that a clinician perform a detailed patient assessment, which typically includes a comprehensive history and examination. Documentation must clearly reflect a moderate to high complexity of medical decision-making, with a focus on the past medical history, current medications, and any pertinent social factors affecting the patient’s health. Additionally, the visit should address multiple chronic conditions or involve a new problem that requires additional workup or discussion, ensuring the visit is appropriately characterized as Level 4 based on the extent of the services provided.
To accurately code for a Level 4 Office Visit CPT, it is essential to adhere to specific time thresholds, usually requiring a minimum of 45 minutes of total time spent on the date of the encounter, including both face-to-face and non-face-to-face activities. Comprehensive documentation is crucial, as it supports the complexity of the visit by detailing clinical reasoning, care coordination efforts, and any patient education provided. Ensuring that all elements are thoroughly recorded not only aids in compliance with coding guidelines but also enhances the likelihood of appropriate reimbursement for services rendered.
– Best Practices for Accurate Reimbursement
Maintaining meticulous documentation is vital for ensuring accurate reimbursement for Level 4 Office Visit CPT codes. Providers should consistently include detailed notes that reflect the complexity of the visit, including the patient’s medical history, examination findings, and the rationale for medical decision-making. This not only justifies the coding but also fosters transparency and accountability in the billing process. Utilizing templates can help streamline documentation while ensuring that all necessary components are captured, reducing the risk of audits or claim denials.
Furthermore, staying informed about payer-specific requirements and updates regarding coding guidelines can significantly enhance the accuracy of reimbursement processes. Regular training sessions for staff involved in coding and billing can improve understanding of Level 4 Office Visit CPT criteria, emphasizing the importance of capturing all relevant clinical details. Additionally, utilizing coding software that incorporates updates from the Centers for Medicare & Medicaid Services (CMS) can assist in minimizing errors and maximizing revenue cycle efficiency, ultimately leading to better financial outcomes for practices.
– Common Mistakes to Avoid with Level 4 CPT
One prevalent mistake is failing to adequately document the medical necessity for services rendered during a Level 4 Office Visit CPT. It is crucial for providers to articulate the patient’s condition, the complexity of the problem, and the decision-making involved in treatment plans. Inadequate documentation may lead to claims denials, as payers often scrutinize the rationale behind the level of care provided. Another common error is misinterpreting the criteria for what constitutes a Level 4 visit; providers may overestimate the level of service based on the number of problems addressed rather than the depth of medical decision-making required.
Additionally, relying on generic templates without customizing them to fit individual patient encounters can diminish the quality of documentation. Each visit is unique, and documentation should reflect not only the clinical aspects but also the person-centric factors that influence treatment. Finally, neglecting to review denial patterns related to Level 4 Office Visit CPT coding can result in missed opportunities for improvement. By proactively addressing these common pitfalls, healthcare providers can enhance their coding accuracy and ensure proper reimbursement for the level of care they deliver.
In conclusion, mastering the Level 4 Office Visit CPT code is essential for healthcare providers aiming to optimize their billing practices and ensure appropriate reimbursement. By understanding the specific requirements for documentation, including the medical decision-making complexity and the extent of the history and examination, practitioners can enhance the accuracy of their coding. Additionally, staying informed about payer guidelines and utilizing best practices for documentation can significantly reduce the risk of claim denials and improve overall revenue cycle management. As the healthcare landscape continues to evolve, a thorough grasp of CPT coding will remain a critical component in delivering high-quality patient care while maintaining financial viability.